The economic case for scrapping prescription charges for people with long-term conditions is here!25/5/2018 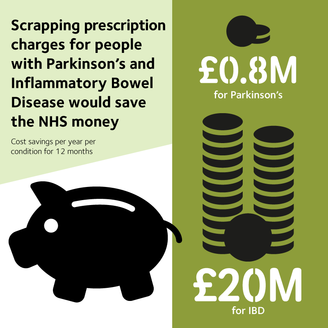 Everyone involved with this campaign has known for a long time that the additional costs to the NHS, resulting from people with long term conditions not taking their medication due to its cost, were likely to outweigh the money raised by charging them for the prescription they need. Thousands of people effectively told us so in our first Paying the Price survey back in 2013 and then again last year in the follow up report Still Paying The Price. Nevertheless, it was still amazing to see the scale of that potential saving to the NHS when the York Health Economics Consortium first shared the findings of their economic modelling with us. Over £20 million per year in NHS savings for just two conditions of the 46 now covered by the Prescription Charges Coalition. This gives us for the first time, a robust economic case for scrapping prescription charges for all long-term conditions. It was fantastic to be able to share this with MPs in Parliament this week (Weds 23rd May). Thanks to the invaluable support from the many people who wrote to their MPs to attend this briefing session, 41 MPs and 3 researchers attended, many of whom were very interested and willing to give their support to the campaign to end unfair prescription charges for people with long-term conditions. Other MPs wrote to express their support and willingness to write to the Minister to call for reform. We now need to build on this. On 5th June, we are handing the petition into Downing Street – please help make this the strongest it can be by signing if you have not already done so and forwarding on to family, friends, work colleagues and anyone you think might be interested. Thank you for all your support and please continue to help us to make prescription charges an issue that can no longer be swept under the carpet. Jackie Glatter, Health Service Development Manager, Crohn's& Colitis UK
0 Comments
 Right now, in the UK, there are about 60,000 people with kidney failure, with just over half alive due a kidney transplant and the remainder on dialysis. Transplant is the gold standard treatment for kidney failure, but not everyone is able to have one and sadly there are more people needing a kidney transplant than there are kidneys available via the organ donor register. Every single day, one person will die while waiting for that precious call. For those 29,000 people on dialysis, they need either to go to hospital three times a week for 3-4 hours at a time for their life-sustaining treatment or they can do this at home. Either way, dialysis is a very challenging treatment. People on dialysis often have other conditions to manage, such as diabetes, and many people will feel unwell during and just after dialysis itself, as blood pressure can be too high or too low, and nausea, fainting and confusion are common. Currently, some dialysis patients will qualify for free prescriptions, but this – rather complicated – exemption is based on the fact that any dialysis patient who has a permanent fistula (which is access for dialysis needles) that ‘requires an appliance or surgical dressing’ is entitled to medical exemption. They also need a doctor to confirm this and the NHS guidance on this even states that ‘whether or not you have a permanent fistula that requires an appliance or surgical dressing is a matter for your doctor's clinical judgement’. This means that in some cases a doctor will approve patients for exemption, but in some cases, they may not – based on their own interpretation of the rules. We have heard from a number of dialysis patients who were able to get exemptions and others who were not, so we know that there is a postcode lottery out there with some patients slipping through the net. If that isn’t bad enough, the injustice really kicks in for those people who do receive that life-transforming transplant. To ensure that your body doesn’t reject your new kidney or kidneys, transplant recipients have to take immunosuppressant medication for the rest of their lives. They also need to take many other medicines to manage blood pressure, diabetes and the other conditions a person with kidney failure will have. Despite this, because they are now no longer on dialysis, they no longer qualify for free prescriptions. At the time when a person possibly needs it the most, this support is taken away. Many patients go on to purchase a Pre-Payment Certificate, but they tell us how unfair it is and how they feel discriminated against, or that they were not aware their exemption was removed and have had to pay a fine. This group are also affected by the recent reports that the NHS will no longer provide sunscreen on prescription, as their immunosuppressants give a risk of skin cancer which is six times higher than the rest of the population. It is not fair that anyone with a long term health condition should have to pay for their prescriptions and we think the current system is particularly unfair for kidney patients, who need to take medication for the rest of their lives, just to stay alive. We’re calling on the Government to review and reform this unjust and outdated system to make prescriptions free for everyone living with a long-term condition in England, as they are in other parts of the United Kingdom. here to edit. Fiona Loud, Policy Director at Kidney Care UK “There have been a few times where I have had to skip my inhaler because I have not been able to afford it. I can't understand why my brother gets his diabetes medication for free but I have to pay for mine despite being hospitalised numerous times because of my asthma?” Asthma UK Facebook post There is nothing as frightening as not being able to breathe, yet this is the reality for someone in the UK every eight minutes as they are admitted to hospital for an asthma attack. Asthma affects 1 in 11 people in the UK and tragically kills around 1,200 every year – that’s three people every day. Those living with this long-term condition often need to take several medicines every day to stay well. Asthma often affects people over their whole lifetime – from childhood to old age. Despite being a complex condition, we know that when people are supported to self-manage their asthma there is significant improvement in their medicine adherence, asthma control and quality of life. Better self-management may result in fewer GP appointments, thus also reducing the 70,000 asthma emergency admissions every year in the UK and saving the NHS money. While we know the NHS faces difficult times, it is unacceptable that 35% of people with asthma receive only the very basic elements of asthma management. Paying for medicines is a real issue, with 64% of people with asthma saying that the charges impact their finances. Now is the time The costs associated with asthma are increasing globally. The UK alone spends in excess of £1 billion in direct healthcare expenditure on the condition. 85% of asthma patients are managed exclusively in primary care, with asthma estimated to account for around 2–3% of GP consultations. Asthma is also estimated to cost around £52m in GP consultations. This comes at a time when GPs are under significant pressure, thus affecting patients and impacting on the wider NHS. Over the years, prescription charges have risen at levels higher than inflation and now represent a significant expense for people with asthma. This year sees the 50th anniversary of the list of conditions exempt from paying for prescriptions. Many conditions that people now live with for years either did not exist when the exemption criteria was created, or had such a short life expectancy that it was thought unnecessary to include them. Despite great medical advances in healthcare, the NHS’s medical exemption criteria for prescription charges has barely changed since its introduction. This level of progress is unacceptable and it’s time for a change. How will this impact people with asthma? 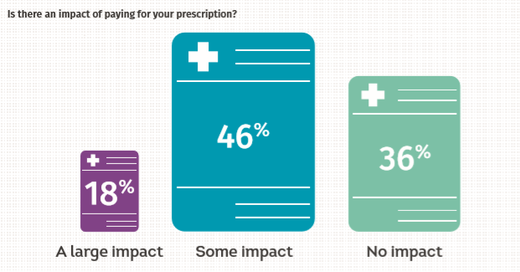 In our recent annual asthma survey, nearly two thirds of people with asthma told us that the cost of paying for their prescription had an impact on them. For some this means the cost of prescriptions prevents them from taking their medicines, forces them to take them in lower doses than prescribed or makes them choose between emergency inhalers and those that prevent future symptoms and attacks. These sacrifices put people with asthma at greater risk of a potentially life-threatening asthma attack. A flexible and fairer approach to prescription charges for people with asthma will benefit those who have been stung by rises in prescription charges in recent years and are struggling to pay for vital medication. Join the campaign today by signing this petition to call on the Government to urgently reform the prescription charge exemption criteria in England. Derry Begho, External Affairs and Stakeholder Officer, Asthma UK |
ActivityHere you'll find information about the Prescription Charges Coalition's latest activities Archives
June 2024
Categories |




 RSS Feed
RSS Feed